Kegel exercises the Kegel is a unique opportunity to train pubococcygeus muscle as recommended by the author.
Around the kegels goes very much speculation.
Very often the "kegels" are called all sorts of gymnastics, which has no relation to the Pins.
When performing Kegel exercises do not have the gymnastic techniques with muscle tension in the abdomen or buttocks or legs, etc., the body's position in space does not change. Most importantly, the pins did not recommend any exercises STRAINING. As for all kinds of devices, the Kegel suggested the use of perineometer and all the modern fixtures have nothing to do with the name of Arnold Kegel. Feature of Kegel exercises that required a GYNECOLOGIST, instructor at first. Without the help of a gynecologist, the patient can not independently determine to feel which muscle you need to train.
So, to be clear, what actually recommended the Kegel — read translation of the article:
A new method of diagnosis and non-surgical treatment in the initial stages of the pelvic organs.
Dr. Arnold Kegel
About a third of all women suffer from a varying degree of relaxation of the pelvic floor. This phenomenon depending on the severity is usually described as a weak perineum, cystocele, rectocele, uterine prolapse - these are all symptoms of an inadequate condition of the neuro muscular apparatus of the pelvic. All this is accompanied by many complications, including inflammatory disease and in previously healthy women. A minor degree of prolapse is not an indication for surgical treatment and women experience discomfort in the flourishing age. Early diagnosis and fiziologicheskaya therapy, consisting of training and practice gives encouraging results .
Introduction
For early diagnosis and successful treatment of minor prolapse of the genitals were surveyed 3,000 women. The condition of prolapse of the genitals was found in women after normal and complicated deliveries, with modern obstetric aid, after caesarean section, and primiparous, and even virgins.
The presence of childbirth in history was otalkuser factor, however, was not a mandatory condition of prolapse of the genitals.
There are many women with a good condition of the pelvic muscles, as a virgin, even after re-delivery or after a difficult delivery.
A large number of women surveyed suggests that nulliparous women and mothers are equally likely to have complaints of pelvic discomfort, urinary incontinence and sexual dysfunction.
Certainly, childbirth and menopause was a predisposing factor for early symptoms or their worsening. Initially, most women have minimal complaints, as they progression of women start to believe that this is a common fee for motherhood.
Examination of the pelvis
Introducing non-surgical method of therapy, it must be emphasized that in the examination of the pelvis has features.
Used to women to confirm the diagnosis the doctor suggested will potushitsya to determine the degree of cystocele, rectocele, and prolapse of the genitals. This was justified because there was no other treatment methods in addition to the pessary, and surgical treatment.
Now offering non-surgical method of treatment, we ask a woman to suck their organs, because we need to determine how impaired muscular function.
So we can assess the potential functional reserve, which we will need in the course of therapy.
External examination
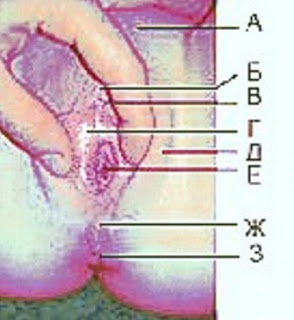
The first stage is external examination, which is carried out on the gynecological chair
In women with prolapse of the pelvic floor is marked sagging of the perineum, dehiscence of the vulva between the buttocks, exposure of the vaginal mucosa and eversion of the anus,
At an early stage, these features are less pronounced. Women of both groups cannot retract the perineum.
A study with a single finger
The second stage — vaginal examination with one finger.
Two-finger palpation of the tissues of the vaginal canal under tension-tension distorts anatomical correlation. The mirror is not used since it is important to examine the middle third of the vagina.
Any reductions in the middle third of the vagina, between the entrance of the vagina and neck usually occur with the participation of the pubococcygeus muscle is a key muscle of the pelvis. This is usually the strongest muscle of the female pelvis. Pubococcygeus muscle surrounds the neck of the bladder, the middle part of the vagina and the rectum, and gives a bit of fine fibers of the internal organs.
Using the index finger need to find the bottom edge of the pubic coccygeal muscle which is palpable at a distance of 1-2 cm from the entrance of the vagina, its position is determined by the tension from the beginning to the frontal bone until it ends at the tailbone. Muscle can be felt if you ask the patient to strain the pelvic floor. Normal thickness of the muscle 3 cm And in patients with weakening of the pelvic floor this muscle can be as thick as a pencil.
In the area where reductions can be identified palpated the position of the pubococcygeus muscle. In the normal state of the pelvic floor, reduction is defined in the lower and in the upper segment, and at relaxation muscle the bag hangs like a hammock, supporting the urogenital diaphragm and the only thing you can feel is a reduction in the gate area of the vagina.
Perineometry
Contractions of pubococcygeus muscle can be assessed by palpation with two fingers, or more accurately using perineometry. Power reduction 5 mm Hg — evidence of the weakness of reduction, against 20-50 mm in normal with good muscle development. The mean values correspond to the edge state. The survey is discussed with the patient to clarify the degree of discomfort and to determine further tactics of training and exercises.
Physiological therapy
In all cases of weakening of the pelvic floor shows the physiological therapy that can be used for prophylactic, curative or for palliation or as an adjunct to surgical treatment or the wearing of a pessary.
As a preventative measure or for therapeutic purposes physiological treatment in any period of woman's life, but is especially recommended for newlyweds, during pregnancy, after childbirth and during menopause.
Even in advanced cases, muscle tissue is and means can successfully be trained.
Surgical treatment is used when the hernia of the perineum, prolapse of the bladder and rectum and in case of advanced genital prolapse. In the preoperative period physiological therapy helps to increase the number and quality of the muscle fibers and reduce the amount of interference, physiological therapy in the postoperative period facilitates early rehabilitation and recovery of function of the pelvic floor, and prevents the recurrence of genital prolapse. Pessaries during physiological therapy can be reversed, and contraceptive rings decrease in size.
Non-surgical treatment of genital relaxation and demonstrations focused on the training of the pubic coccygeal muscle
Impressive that improvement is achieved by training a single muscle. Also improves the function of the sphincters and sexual function is restored.
Muscle training.
At the first stage of physiological therapy is "training" the muscles.
A woman with genital prolapse has problem with pubic-PC muscle and you have to learn to define (to feel) this muscle. Instructions how to develop the muscle function through its own efforts.
At the time when the patient produces contraction of the pelvic floor muscles, the physician positions the tip of your finger on pubococcygeus muscle and every time he feels the reduction, it shall inform the patient, giving her some cuts efficient which are not. "That's right! Please remember this acronym! Do this exercise many times a day, while the bodies will be in place".
The patient should not do any effort other muscles, including should not reduces the muscles of the buttocks or stomach or chest muscles!
The use of perineometry. After 5-10 correct reduction perineometer is introduced into the vagina and the doctor together with the patient see the gauge and strength of contractions. A woman can practice the exercises with the apparatus in the treatment room for 5-10 minutes, while the doctor checks the correctness of reductions and gives instructions.
Exercises perineometry used in order to:
- To acquire the positive result without delay.
- To restore the function of the pubic coccygeal muscle to the level of healthy women.
- Develop the power of many small muscle fibers concentrate Czech and lateral to these muscle fibers worked together with the main muscle , rather than building her resistance.
The basic physiological principle that muscle will increase its force only at repeated repetition of exercises. The woman, seeing the results day by day on the manometer, and inspired to continue the exercise.
The patient should work with perineometer 20 minutes two or three times a day.
To quickly reach the woman and without perineometer to exercise its muscle 5 to 10 times every half hour, and also to do exercise to interrupt urination several times a day, whenever she urinates.
Women with genital relaxation and having fascial support in the pelvis is muscular, over the years you get used to and their feelings and consider their pelvic floor normal. In addition, in order to accustom the patient to the new sensations of muscular support, it is recommended to raise the crotch a few times in the morning before she got up out of bed and start the day with pull-UPS of the perineum and hold it in this position.
This daily morning ceremony should become a habit, feeling elevated and held in this condition, the perineum should be unconditional reflex without any external force.
The survey shows that such exercises are much more effective than surgery to repair the fascia.
The subsequent examination.
Subsequent medical examination should be carried out at intervals of 1 to 3 weeks . Approximately 75% of patients reported the successful use of the exercise and reduce the symptoms within a few weeks.
When the patient is lying down, the exercise by pulling and holding the crotch should be repeated , especially at home and with the registration success on perineometry or perform this exercise without perineometer. This gives the physician the opportunity to monitor the result of the exercise pubococcygeus muscle. This is an additional encouraging sign that the patient may perform the movement of the perineum and bladder control or to tighten the bladder in cystocele at each exercise — reducing.
Fingertip doctor has consistently in the lower segment , the middle segment and the top segment of the pubic coccygeal muscle and acknowledges tone, tension, thickness of the muscle. Perineometer records the strength of the contractions. Usually registers a pressure increase on the 1-5 mm in comparison with the results of the first visit, if the exercises are done correctly. However, if the pressure suddenly rises to 20 mm above and this is indicative that the patient is using accessory muscles.
Volume of exercise is not limited, the more correct cuts would be made, the faster and more stable result will be obtained, and a new reflex becomes a habit, "I make cuts and tighten the crotch without thinking about it."
If during the second or third visit, the patient noted improvement or examination does not show early signs of improvement, it is immediately discussed: or the woman persists in its exercise, or straining the wrong muscles. In cases of muscle fatigue, it is evident after 3 or 4 cuts.
An interesting observation that in the case of incontinence and dyspareunia in women are more Executive than in the case of border States.
Complications with the treatment.
If a woman complains that she found it difficult to do the exercises that she has tired muscles or increased nervousness, you need to ask her to demonstrate how she performs exercises at home, she probably wrong tenses with involvement of the abdominal muscles, buttocks, lower back and even the respiratory diaphragm. Dizziness may be, if a woman engages in muscle, makes the breath-hold. The most dangerous symptom is the fulfillment naturewise instead of just pulling the crotch, POI all the symptoms of prolapse can worsen.
Approximately 15% of women incorrectly find yourself pubic coccygeal muscle and in that case you have to repeat the instruction. These women are encouraged to focus home exercises to stop urinating or the idea that they control the urge to use the toilet.
If a woman is able to combine arbitrary acronyms with the effort usual for her, you can be sure that it uses at least a portion of pubococcygeus muscle. As soon as will achieve minimal contraction of this muscle, the patient can be transferred to regular homework sessions with perineometer or without him. The duration of training and the efforts depend on how pronounced were the symptoms initially.
When there is a break after a difficult childbirth or operations in the pelvis , it is possible that the muscle flap was sewn to the fascia with the formation of fibrosis. Fascia is not as elastic as the murine tissue, but in this case, a regular exercise program can achieve significant progress.
Results.
The result of muscle training, performed correctly, is interesting from a clinical and from a scientific point of view. It shows that there is a connection between the support function of the pelvis, the function of the sphincters, sexual function and have their interactions, also have the control of motility and sensitivity. Instead of the usual practice of treating all these disorders separately, a new method of treatment of the soft tissues of the pelvis, neuromuscular units, allows you to achieve the best results in General, the treatment of certain disorders.
With improved support functions of the pubococcygeus muscle of the pelvic floor lifted (it provides a permanent effect), it pulls all the pelvic organs and their sphincters in a more physiological state. The sphincters of the vagina, urethra and rectum are also beginning to act more consistently, sexual function is improved by lengthening and narrowing of the vagina, improves the contact and sensitivity of the vagina. Patients report improved sexual sensations and relief from discomfort during sexual intercourse. Is enhanced and vaginal orgasm.
Improved circulation as a result of the training leads to a decrease of stagnation in the pelvis, which is accompanied by improved hydration of the mucous membranes and the reduction of the residual tension in the muscles of the pelvic floor.
In this clinical study, special attention was paid to the early symptoms of genital prolapse, as training therapy can improve quality of life of women flourishing age.
The development of genital prolapse coincides with certain eras in a woman's life when the signs of prolapse first can be spotted and alleviated:
Adolescence and early adulthood — symptoms of insolvency of the bladder.
Early marital period, sexual dysfunction and pain during urination
During pregnancy
Weak muscle tone in the pelvis
Loss of function of the pubic coccygeal muscle
The inability to create pressure in the vagina more than 5 mm Hg.PT.
In the period after birth
Delay uterine contractions with or without bleeding,
Incomplete recovery of contractile function of the pelvic muscles, especially in the middle part of the vagina, bladder, rectum and perineum,
Pelvic fatigue, decreased sensitivity,
Violation of sensitivity of the vagina
In adulthood, problems with urinary incontinence, occasional or constant nocturia — may be an early symptom of degenerative processes in the pelvis that can be prevented with exercise.
The amount of restored function of the female pelvis, as one of education, confirmed positive obstetric and urological observations.
The effectiveness of antenatal exercises described by Bushnell in monitoring 800 pregnant women in whom he observed the closure of the vagina in 24 hours after birth, cystocele was noted in any of his patients.
During 1948 in the clinic of the medical faculty of the University of southern California and at the state General hospital of Los Angeles, all the patients with urinary incontinence were examined using perineometry for further physiological therapy. Surgical treatment was deferred for seven years and positive results have been reported by many doctors in the U.S. and other countries. Part they due before surgery were aimed on the physiological treatment and after his adventures in the need for surgery has disappeared.
Conclusions.
The signs and symptoms of General weakening of the pelvic floor can be recognize until the first pregnancy or to the development of degenerative changes during menopause. Total
the weakening is the result of prolonged neuromuscular dysfunction that may be prevented or cured muscle training, except in rare cases muscle injury. Features of the examination , diagnosis and psychological treatment are described.
Other articles describing the Kegel exercises:
Kegel exercises in the article "Nonsurgical treatment of stress urinary incontinence"
1952
Kegel exercises the "non-Surgical treatment of genital prolapse" 1948
Kegel exercises during sexual dysfunction caused by a breach in the pubic coccygeal muscle. 1952
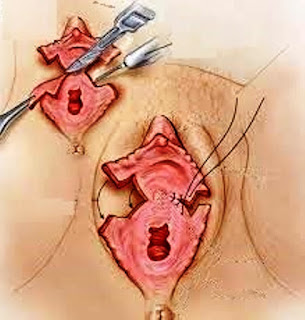
 Overgrown hymen (a hymen in which there is no hole, as a result in the vagina to accumulate blood, the so-called hematocolpos).
Overgrown hymen (a hymen in which there is no hole, as a result in the vagina to accumulate blood, the so-called hematocolpos).